Remember when you had a newborn baby and how sleep-deprived you were? That is how our men with BPH feel all the time; they are awakened multiple times a night to urinate.
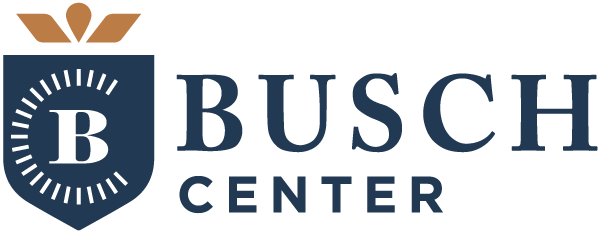
As men age the transitional zone (TZ) of the prostate develops benign prostatic hypertrophy nodules (BPH) which causes the transitional zone to increase in size. Over time, the prostate will start to squeeze the bladder neck which contains the internal sphincter that signals to the man that he needs to urinate.
The prostate is the most abused organ in the man’s body. When the man is sleeping, his rectum fills with stool which pushes the prostate anterior (toward the symphysis pubis) and superior (toward the head). The bladder fills, pushing the prostate down, and when the man rolls over with all this pushing, the anterior or posterior median push on the bladder neck and the internal sphincter signals to the man that he needs to urinate. The prostate is always getting pushed around.
A normal prostate is 30-40 cc (the size of a walnut). The image below shows a prostate size of 223 cc, which is 7-8 times the size of a normal prostate.
Also, the male pelvis is shaped differently from the female pelvis. Because the male pelvis is much narrower and longer, it is more difficult to perform a robotic prostatectomy due to having less area to work with. This stands true when the prostate increases in size. The prostate tries to fill a space that is already filled.

With all this crowding going on in the pelvis it is WONDERFUL that we can offer TULSA treatment of BPH because the other treatments offered today have not worked and some cause more issues than cure.
TREATMENTS for BPH
- TURP. Transurethral Resection of the Prostate (TURP), a combined visual and surgical instrument (resectoscope), is inserted through the urethra where it is surrounded by prostate tissue. An electrical loop cuts away excess prostate tissue to improve urine flow. Results: the bladder falls into the hole created by the TURP and the patient may now have more emptying problems. Also, can cause damage to the urethra from the electrical loop cutting through it to cut the prostate tissue.
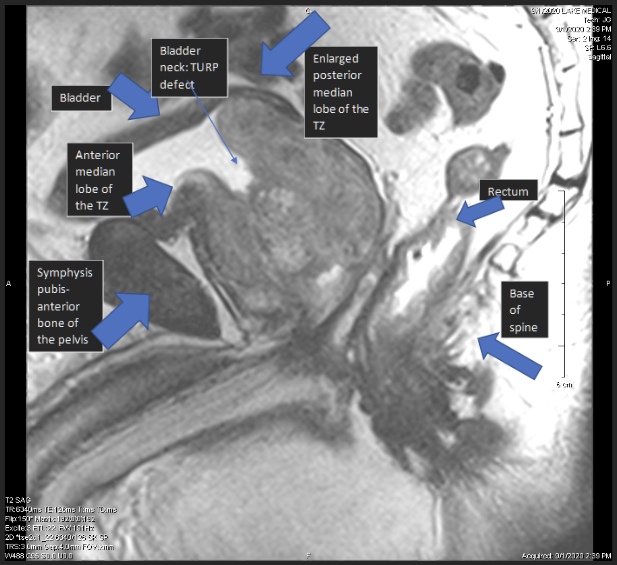
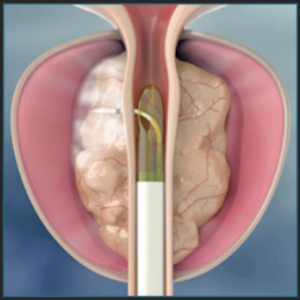
- Urolift. A one-time, in-office procedure that provides rapid relief and recovery of BPH symptoms. The Urolift approach to treating BPH lifts and holds the enlarged prostate tissue so it no longer blocks the urethra. Once the Urolift has been placed in the prostate, the man cannot have a TULSA Procedure due to the metal from the Urolift.
Below is an image of the Urolift in the prostate.
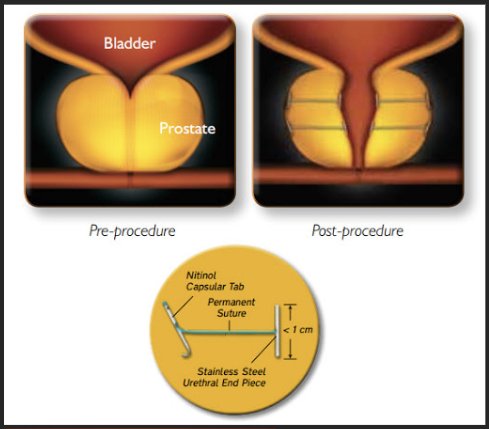
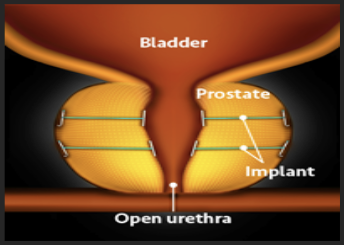
The following images are images of a real patient with Urolift which doesn’t look like the textbook image from the Urolift website.

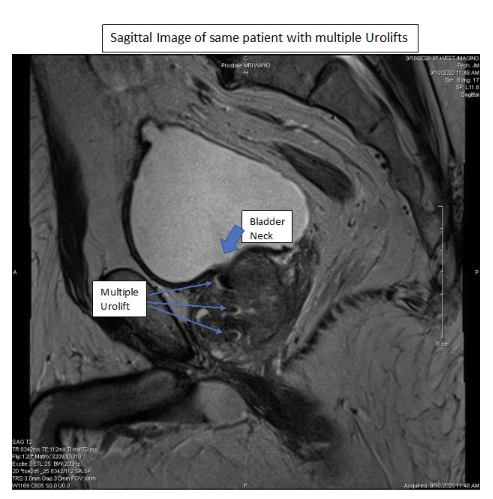
The Urolift is not working very well staying off the urethra. Urologists are paid between $7k-8k for the placement of 1-3 Urolift implants and the maximum prostate size for treatment is less than 100 cc.
- Rezum. A minimally invasive transurethral water vapor therapy for benign prostatic enlargement which uses thermal energy for treatment. The short-term results show it to have good outcomes with the potential for outpatient-based treatment preserving sexual function. The image below shows the water vapor tip piercing the prostate urethra and this happens multiple times depending on the number of treatments.
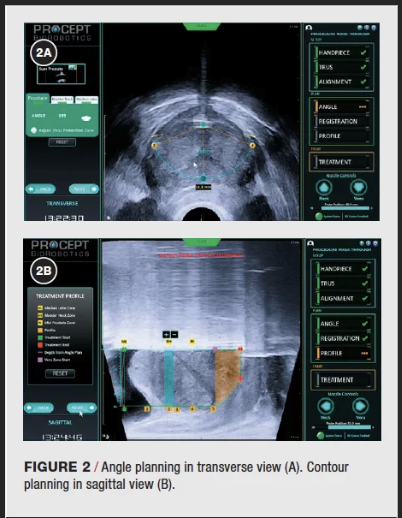
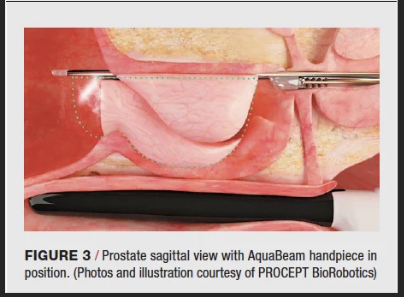
- Aqua Ablation. A minimally invasive surgical technology for benign prostate enlargement, which uses high-pressure saline to remove parenchymal tissue through a heat-free mechanism of hydrodissection. Early results show this to be a promising surgical strategy with a strong morbidity profile and reduced resection time. In 2017, the U.S. Food and Drug Administration (FDA) approved the AquaBeam Robotic System to perform the procedure, known as aquablation (aqua is Latin for “water” and ablation means “to remove” or “reduce in volume”). How it’s performed: After the patient receives general or spinal anesthesia, a handpiece is inserted into the prostatic urethra and secured in place. Using real-time transrectal ultrasound guidance, the surgeon “maps” the area to be treated, sparing the bladder neck and urinary sphincter. The surgeon then triggers the robotically controlled handpiece to release a high-pressure stream of sterile saline to destroy the excess prostate tissue. The stream moves in a controlled manner from the bladder to the end of the prostate (verumontanum). The entire procedure takes less than an hour; the aquablation portion lasts about 10 minutes. An overnight hospital stay is typically required. Nevertheless, the most recent American Urological Association (AUA) guidelines say the treatment can be offered to men with prostates measuring less than 80 cc. TULSA can treat a prostate gland up to 250 cc in size.
Today, urologists use the International Prostate Symptom Score (IPSS) to screen, diagnose, track symptoms, and suggest management of the symptoms for BPH. We also ask the eight questions of our patients. The significance of the IPSS score can determine the severity of their BPH and how often they get up at night. This is very important to the health of the man (sleep).
Wikipedia States:
The International Prostate Symptom Score (IPSS) is an eight-question written screening tool used to screen for, rapidly diagnose, track the symptoms of, and suggest management of the symptoms of benign prostatic hyperplasia (BPH).
It contains seven questions related to symptoms related to BPH and one question related to the patient’s perceived quality of life. Created in 1992 by the American Urological Association, it originally lacked the eighth quality of life question, hence its original name: the American Urological Association symptom score (AUA-7).[1] World Health Organization International Consultation on BPH adopted the “eight question” index and labeled it the IPSS[2].
| IPSS score (out of 35) | |
| Score | Correlation |
| 0-7 | Mildly symptomatic |
| 8-19 | Moderately symptomatic |
| 20-35 | Severely symptomatic |
The seven questions relating to symptoms experienced in the last month include feeling of incomplete bladder emptying, frequency of urination, intermittency of urine stream, urgency of urination, weak stream, straining and waking at night to urinate.[1]
The IPSS was designed to be self-administered by the patient, with speed and ease in mind. Hence, it can be used in both urology clinics as well as the clinics of primary care physicians (i.e. by general practitioners) for the screening and diagnosis of BPH.[1]
Additionally, the IPSS can be performed multiple times to compare the progression of symptoms and their severity over months and years.[1]
In addition to diagnosis and charting disease progression, the IPSS is effective in helping to determine treatment for patients.[1]
In research, the IPSS is used to standardize patients’ complaints and symptoms. However, a meta-analysis on the subject of the influence of position (whether standing or sitting) on urodynamics (that is, on tests of how completely the bladder, sphincter and urethra store and release urine) noted that, in most cases, physicians either did not use the IPSS, or did not use it adequately.[4]
References[edit]
- ^ Jump up to:a b c d e f g h International Prostate Symptom Score (IPSS) at Urological Sciences Research Foundation. Retrieved November 2011
- ^ Cockett, A. T. K. (1992). The International Consultation on Benign Prostatic Hyperplasia. 1991: Paris, France: World Health Organization. ISBN 2905744111.
- ^ http://www.urospec.com/uro/Forms/ipss.pdf
- ^ de Jong, Y; Pinckaers, JH; ten Brinck, RM; Lycklama à Nijeholt, AAB; Dekkers, OM (2014). “Urinating Standing versus Sitting: Position Is of Influence in Men with Prostate Enlargement. A Systematic Review and Meta-Analysis”. PLOS ONE. 9 (7): e101320. doi:10.1371/journal.pone.0101320. PMC 4106761. PMID 25051345.
- 2018 – Elterman – FUS 2019 Poster TULSA BPH
- This is a conference poster from the 6th International Symposium on Focused Ultrasound 2018, in Reason VA, USA.
- Important: This is a sub-group analysis of 9 men from our 30-patient Phase I study in localized prostate cancer patients. These 9 men had IPSS >= 12 before TULSA, in addition to having localized prostate cancer according to the eligibility of our Phase I study for cancer.
- IPSS >= 12 means they have moderate to severe LUTS (lower urinary tract symptoms) but does not mean they were diagnosed with BPH.
- In this subgroup of men, we saw an average 10-point decrease in IPSS which is a similar effect size to Rezum (water vapor) and Urolift.
- This work has been submitted to J Endourol and currently undergoing review. We hope to have it published by the end of this year.
- EAU2020 presentation – Anttinen – BPO
- This is a conference-moderated poster presentation from the 2020 European Association of Urology (virtual)
- This is very early results from a 10-patient clinical trial in Finland, prospectively enrolling BPH patients for treatment with TULSA.
- Patients had a baseline IPSS 17.7 (Moderate) and at 3 months follow up 4.6 (mildly symptomatic)
- The decrease, so far, in IPSS is greater (better) than what we showed in the sub-group analysis above.
- Patients at baseline average urine flow rate ml/sec (better stream) baseline 5.6 ml/sec and 3 months 11.3 ml/sec
- Patients residual volume (ml) at baseline 245 ml after urinating and at 3 months post 84 ml.
Hopefully, this will help explain why TULSA is so important for BPH treatment.