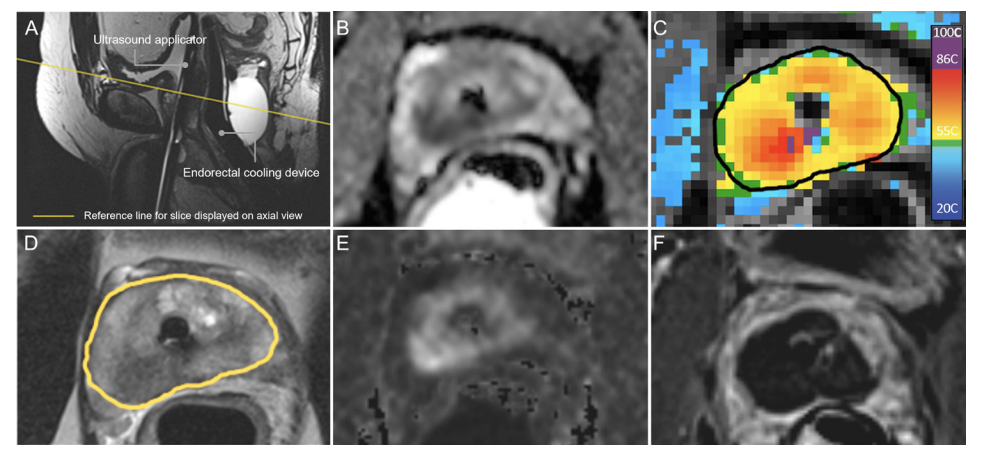
Prostate cancer continues to have a negative impact on the duration and quality of life for males and their families. MRI is transforming the pathway of prostate cancer detection, diagnosis, staging, and surveillance, backed by multiple Level 1 studies and robust reporting standards. This evolving paradigm of MRI-directed care is now being expanded to include in-bore MRI-guided prostate tissue ablation techniques, which reduce the burden of genitourinary complications associated with standard-of-care treatments, without sacrificing cancer control. The workflow for MRI-guided transurethral ultrasound ablation relies on intraprocedural MRI guidance for treatment planning, automated and physician-monitored treatment delivery, and post-treatment assessment at both immediate and long-term time points. Our early experience has identified several procedure refinements, and aligns with early evidence from prospective clinical studies using transurethral ultrasound ablation for treatment of patients with either primary or recurrent disease. Driven by quantitative real-time imaging, MRI-guided ablative interventions provide rich datasets for developing technical refinements and predictive models that will progressively improve patient outcomes as these novel techniques become part of a new standard-of-care.
Read more about our TULSA findings and the innovation of prostate cancer treatment in this paper, The role for MRI-guided transurethral ultrasound ablation in the continuum of prostate cancer care by Dr. Joseph Busch, originally published by the British Institute of Radiology.